|
Healthy eating can reduce your risk of stroke. Aim to eat a wide variety of healthy foods. Using the Food Pyramid can help make sure you get all the vitamins, minerals, fibre and goodness you need.
Some tips to help family and friends cope with a loved one's stroke:

Adaptive equipment can be used to help stroke patients have greater independence with everyday life skills or activities of daily living. There is a great assortment of assistive devices for all areas of self care including dressing, bathing, grooming, cooking, feeding, toileting, and mobility aids. There are also assistive technology devices to help with communication, using a computer, operating household devices, and driving.
Various medical and personal care equipment choices can be found below. If interested in purchasing any of the adaptive equipment, you can visit websites such as www.activeforever.com, www.wayfair.com, and www.pattersonmedical.com. Make sure you know the return policy before ordering any equipment. Many types of medical and bathroom equipment items are non-returnable due to sanitary reasons. This means you should research equipment before buying and make sure it is the right equipment for you, has good reviews, and will fit in the space needed if applicable. If you are interested in finding clothing for a stroke patient which allows for easier dressing such as donning pants from a seated position, please visit this adaptive clothing page. You can also search Amazon.com and other similar websites to compare prices and get the best deal on adaptive equipment. Donating or Finding Used Equipment If you have medical or adaptive equipment that you no longer need, you can search the term "donate DME" on the internet to find local DME (durable medical equipment) exchanges or non-profits that will take your equipment to be used for others in need. You can also use that same search term if you cannot afford equipment and want to find a local business that offers inexpensive prices or free DME for those who qualify. Mobility Devices:
Rolling Walkers - If the stroke victim has use of both arms and legs but still presents with some balance problems or slight weakness then a rolling walker may be appropriate. One must be able to push forward with both arms to operate a rolling walker. The most common are 2 wheel walkers, 4 wheel walkers and rollators (4 wheel walker with a seat).
Hemi-Walkers and Quad Canes - When the stroke victim is paralyzed and does not have good use of one side such in the case of hemiplegia or hemiparesis, then a hemi-walker or quad cane may be needed. These types of mobility aids have a wider base of support than a single tip cane thus providing more support but not requiring the use of both hands to operate.
Quad canes come with small or large base depending on the amount of support needed. One drawback to a hemi-walker or quad cane is that the stroke victim mostly relies on the non-affected side for walking and does not incorporate using the weak side as much so one must remember to continue working on exercises and weightbearing to the weak side to prevent neglecting these muscles.
Single Tip Canes - If the stroke patient only needs minimal support for steadying, then a single tip cane may be appropriate.
Wheelchairs and Scooters - Many stroke victims will need a wheelchair due to limited mobility. A hemi wheelchair is a special wheelchair which can be adjusted lower to the ground and allow the ability to operate it with one or both feet. Electric wheelchairs and scooters are also available some which can be operated with one hand.
Bathroom Aids
Shower Chairs and Tub Benches - Shower chairs with and without backs can be purchased for walk-in showers or bathtubs. For the stroke patient that has a bathtub and cannot step over the side, a transfer tub bench that extends over the side would be more appropriate. Hand-held showers can also be purchased to make showering from a seated position more convenient. Toilet Seats and Bedside Commodes - Raised toilet seats or toilet seats with handles can be purchased to make standing up from the toilet easier. If the bathroom is not accessible or the stroke patient needs the convenience of a toilet next to their bed then a bedside commode can be used.
Other Bathing/Dressing Aids - Various adaptive equipment exists to make bathing amd dressomg easier for stroke victims such as a bathing mitt, hair shampoo tray, long-handled sponge, reachers, long shoehorns, sock aids, elastic shoelaces, dressing sticks, button hooks, and more:
Hospital Beds Electric hospital beds make it easier to get a person out of bed or to sit a person up in bed. This can become important for the stroke patient who has a peg tube and swallowing difficulties that require the head of the bed to be raised. It also is helpful for caregivers taking care of stroke patients with limited mobility.
Kitchen Aids - A variety of one handed devices exist for people to use in the kitchen such as one handed cheese slicers, rocker knives, cutting boards with suction cups, and scoop plates:
Grooming Aids Devices used to help with grooming include brushes with suction cups, hair dryer racks, toothpaste squeezers, and various utensils with adapted handles.
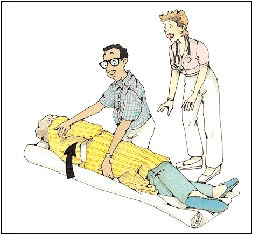
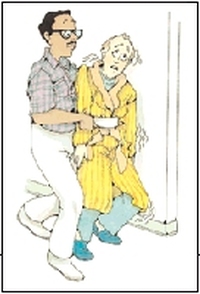 Once the momentum has started, it’s almost impossible to stop a patient from falling. By trying to do so, you can injure your back. Instead, guide the patient to the ground; then get help to move the patient back to a bed or stretcher. Guiding the Fall Help falling patients to the floor with as little impact as possible. If you’re near a wall, gently push the patient against it to slow the fall. If you can, move close enough to “hug” the patient. Focus on protecting the patient’s head as you move down to the floor. Then call for help. Blanket under patient Moving a Fallen Patient Patients who’ve fallen may feel dizzy or faint. Reassure them as you determine whether they’ve been injured. If so, tend to the injury before doing anything else. If the patient isn’t injured, you can prepare for the move back to a bed or stretcher. Get help. Four or more people may be needed. 1 Roll onto Blanket
Palms up 2 Lift from Floor
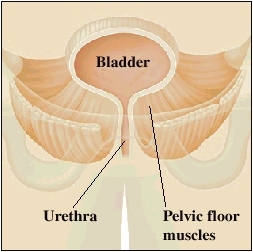 A weak pelvic floor The pelvic floor muscles may weaken due to aging, pregnancy and vaginal childbirth, injury, surgery, chronic cough, or lack of exercise. If the pelvic floor is weak, your bladder and other pelvic organs may sag out of place. The urethra may also open too easily and allow urine to leak out. Kegel exercises can help you strengthen your pelvic floor muscles. Then they can better support the pelvic organs and control urine flow. How Kegel exercises are done Try each of the Kegel exercises described below. When you’re doing them, try not to move your leg, buttock, or stomach muscles.
Try to hold each Kegel for a slow count to 5. You probably won’t be able to hold them for that long at first. But keep practicing. It will get easier as your pelvic floor gets stronger. Eventually, special weights that you place in your vagina may be recommended to help make your Kegels even more effective. Visit your healthcare provider if you have difficulties doing Kegel exercises. Helpful hints Here are some tips to follow: · Do your Kegels as often as you can. The more you do them, the faster you’ll feel the results. · Pick an activity you do often as a reminder. For instance, do your Kegels every time you sit down. · Tighten your pelvic floor before you sneeze, get up from a chair, cough, laugh, or lift. This protects your pelvic floor from injury and can help prevent urine leakage. .
Larynx-closure exercises can help you swallow better. They are used if you have trouble swallowing (dysphagia). Your larynx is the part of your throat that is also known as your voice box. Swallowing exercises can improve the strength and control of these muscles, and how well they move. Over time, they may help you to swallow normally again.
A speech-language pathologist (SLP) may prescribe swallowing exercises to improve your swallowing. You can do these exercises in your hospital room or at home. Often you can do these exercises on your own. But you may also work with a health professional to practice them. How swallowing works Before you swallow, you chew your food to an appropriate size, shape, and texture. When you swallow, this material passes through your mouth and a part of your throat called the pharynx. From there the chewed food goes through a long tube called the esophagus. It then enters your stomach and your digestive tract (gastrointestinal tract). During breathing, air travels from your mouth and pharynx into the larynx (toward your lungs). When you swallow, a flap called the epiglottis moves to stop any food particles from entering your larynx and lungs. The muscles of the larynx pull upward to help with this movement. They also tightly close during swallowing. That prevents food from going into your lungs. Swallowing requires the muscles in these regions to work together. But sometimes they may not work right. That can lead to problems swallowing. Muscle weakness in these areas can make swallowing hard to do. For example, food particles might be more likely to end up in your lungs if the muscles that close your larynx are weak. When closure of the larynx exercises are needed You might need to do larynx-closing exercises if you have trouble swallowing. Not being able to swallow properly is called dysphagia. Dysphagia may lead to aspiration. That’s when material from your stomach and intestines enters into your airways. This serious situation can lead to pneumonia and other problems. As a result dysphagia should be diagnosed and treated as soon as possible. Different conditions can cause swallowing problems. Some examples are:
Before you start these exercises, you may need to be standing or sitting in a chair. Your SLP will show you what to do. For example, it may be better if you do these exercises while out of bed. It is best to remove distractions from your environment. Turn off the television. Do the exercises at a time when you won’t have visitors. You will be able to fully concentrate and get the most benefit from them. You can do these exercises at any time that is convenient for you. Sample exercises Your SLP can show you the specific exercises you should do and explain how often to do them. As an example, you may be asked to do these exercises:
All of these exercises help close the larynx. That may improve your swallowing. In most cases, you’ll be practicing the larynx-closing exercises along with other types of swallowing exercises. If so, do these in the same order each time. Don’t leave any exercises out. Your health care team will plan a series of exercises that specifically targets the source of your swallowing problem. Keeping track of your progress Keep a record of the times you do your swallowing exercises. It will remind you to do your exercises as prescribed. It will also provide helpful feedback on your progress to your SLP. Make a note of what exercises you do and when you did them. Also note any problems. Discuss them with your SLP. Your SLP and medical team will watch your progress. They may make changes to your exercise therapy, if needed. This monitoring may include bedside swallowing exams or imaging tests. It may take a few weeks to notice that your swallowing is better. As your ability to swallow gets better, your risk for aspiration may drop. Your SLP may be able to modify your diet. You may also be able to eat certain types of food again. This can improve your nutrition, your overall health, and your quality of life. Continue to practice all your swallowing exercises as prescribed by your SLP. You will benefit most from following the prescribed therapy. Your gains may be less if you miss practice sessions. To make it more likely for you to succeed, work closely with all the members of your health care team to properly treat your condition.  Doing special exercises is the first way to treat frozen shoulder. You may see a physical therapist who can help you learn to do them. If these exercises don’t help, you may need further medical treatment. Shoulder stretches Doing stretches is often the best way to treat frozen shoulder. Stretching each day can help lessen the pain and restore shoulder flexibility. But it often takes time before you notice results. Try to be patient. To warm up, do the “pendulum.” While standing, let the hand on your frozen side dangle freely as you hold the back of a chair with your other hand. Slowly make circles and side-to-side motions with the frozen arm. Physical therapy Your doctor may refer you to physical therapy. This hands-on care helps you learn how to do stretching exercises at home. A physical therapist may also work on restoring your shoulder flexibility. To do this, he or she may gently stretch and move your frozen shoulder. Tips for shoulder stretches
|
STROKE REHAB CORNER
This blog provides info on many rehab activities that stroke patients face. You may have to do your own independent home rehab, so use this information ONLY as a guide. Please consult with your doctor before starting any rehab exercise activity. Archives
January 2019
Categories
All
|
























 RSS Feed
RSS Feed