Left Hemispheric Stroke
WHAT YOU NEED TO KNOW:
What is a left hemispheric stroke?
A stroke happens when blood cannot flow to your brain. A stroke caused by a blood clot is called an ischemic stroke. A stroke caused by a burst or torn blood vessel is called a hemorrhagic stroke. When stroke symptoms last a few minutes to hours and do not cause damage, it is called a transient ischemic attack (TIA). A TIA is a warning sign that you are at risk of soon having a stroke.
What are the signs and symptoms of a left hemispheric stroke?
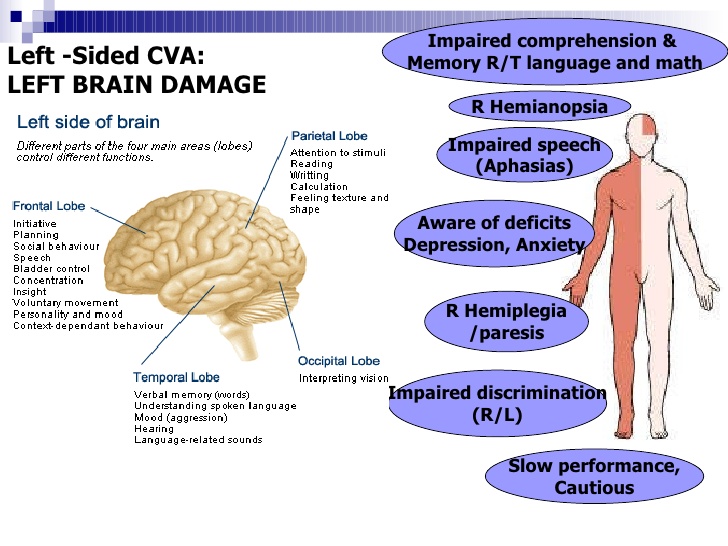
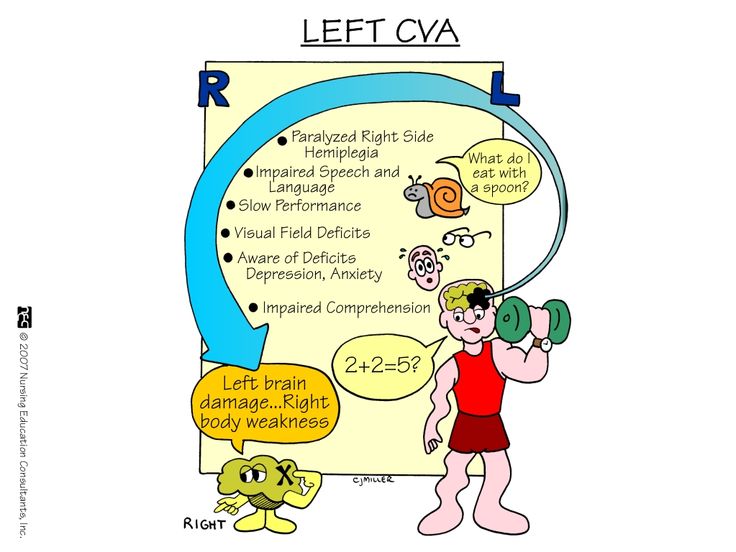
The left hemisphere (side) of your brain controls the right side of your body. It also controls your speech and language abilities. You may have any of the following:
What are the warning signs of a stroke?
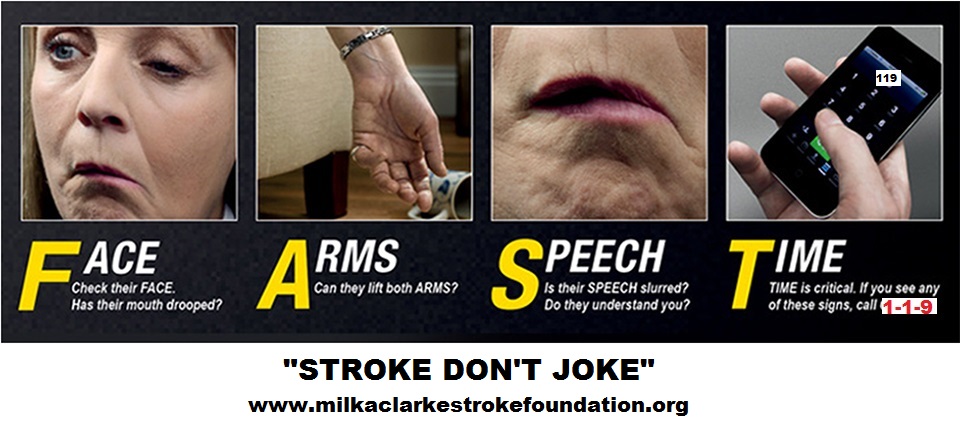
The word F.A.S.T. can help you remember and recognize signs of a stroke:
What increases my risk for a left hemispheric stroke?
How is a left hemispheric stroke diagnosed?
Your healthcare provider will ask about your symptoms and when they started. He will look for signs that show which part of your brain was injured. You may need any of the following:
How is a left hemispheric stroke treated?
What is a left hemispheric stroke?
A stroke happens when blood cannot flow to your brain. A stroke caused by a blood clot is called an ischemic stroke. A stroke caused by a burst or torn blood vessel is called a hemorrhagic stroke. When stroke symptoms last a few minutes to hours and do not cause damage, it is called a transient ischemic attack (TIA). A TIA is a warning sign that you are at risk of soon having a stroke.
What are the signs and symptoms of a left hemispheric stroke?
The left hemisphere (side) of your brain controls the right side of your body. It also controls your speech and language abilities. You may have any of the following:
- Trouble swallowing, walking, or remembering
- Paralysis or weakness on the right side of your body
- Falling toward your right side
- Lack of awareness of the right side of your body
- Trouble speaking, reading, writing, or understanding language
- Changes in mood or the ability to pay attention or learn new information
What are the warning signs of a stroke?
The word F.A.S.T. can help you remember and recognize signs of a stroke:
- F = Face: One side of the face droops.
- A = Arms: One arm starts to drop when both arms are raised.
- S = Speech: Speech is slurred or sounds different than usual.
- T = Time: A person who is having a stroke needs to be seen immediately. A stroke is a medical emergency that needs immediate treatment. Some medicines and treatments work best if given within a few hours of a stroke.
What increases my risk for a left hemispheric stroke?
- Age 55 or older
- Being male or African American
- Physical inactivity or obesity
- High cholesterol, high blood pressure, or diabetes
- Smoking cigarettes or using illegal drugs such as cocaine
- Chronic inflammatory disease, such as rheumatoid arthritis or lupus
- A family history of stroke, or a low birthweight
- A heart condition such as atrial fibrillation, myocardial infarction, or valve disease
- Birth control pills or hormone replacement medicine (women)
- Current pregnancy, or delivery within the past 6 weeks
How is a left hemispheric stroke diagnosed?
Your healthcare provider will ask about your symptoms and when they started. He will look for signs that show which part of your brain was injured. You may need any of the following:
- CT or MRI pictures may show where the stroke happened and any damage to your brain. You may be given contrast liquid to help your skull and brain show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- An arteriography is used to take x-rays of your arteries to look for blood flow blockage.
- A carotid ultrasound may show narrow or blocked carotid arteries. The carotid arteries are blood vessels in your neck that carry blood to your brain.
How is a left hemispheric stroke treated?
- Medicines may help improve your blood's ability to clot and stop the bleeding. You may instead need medicine to break up blood clots, or to prevent them from forming. The type of medicine you receive depends on what is causing your stroke. You may also need medicine for high blood pressure, high cholesterol, or diabetes.
- Thrombolysis is a procedure used to break apart clots in an artery. A catheter is guided into the artery until it is near the clot. Medicine is put through the catheter that will help break apart the clot. The clot may be pulled out of the artery during the procedure.
- Surgery may be used to remove a blood clot or to relieve pressure within your brain. You may also need surgery to remove plaque buildup from your carotid arteries.
What is rehabilitation (rehab)?
Rehab is an important part of treatment. A speech therapist helps you relearn or improve your ability to talk and swallow. You may start slowly and start doing more difficult tasks over time. Physical therapists can help you gain strength and build endurance. Occupational therapists teach you new ways to do daily activities, such as getting dressed. Therapy can help you improve your ability to walk or keep your balance. Your therapy may include tasks or movements you will need to do for everyday activities. An example is being able to raise or lower yourself from a chair.
How can I decrease my risk for a stroke?
Call 119 for any of the following:
When should I seek immediate care?
When should I contact my healthcare provider?
Rehab is an important part of treatment. A speech therapist helps you relearn or improve your ability to talk and swallow. You may start slowly and start doing more difficult tasks over time. Physical therapists can help you gain strength and build endurance. Occupational therapists teach you new ways to do daily activities, such as getting dressed. Therapy can help you improve your ability to walk or keep your balance. Your therapy may include tasks or movements you will need to do for everyday activities. An example is being able to raise or lower yourself from a chair.
How can I decrease my risk for a stroke?
- Do not smoke cigarettes or use illegal drugs. Smoking and drugs increase your risk for a stroke. Nicotine and other chemicals in cigarettes and cigars can cause blood vessel damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Limit or do not drink alcohol. Heavy alcohol use or drinking binges increase your risk for any type of stroke. Limit alcohol to 2 drinks per day if you are a man. Limit alcohol to 1 drink per day if you are a woman. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Manage health conditions. Take your medicine as directed. Check your blood pressure and blood sugar levels as directed. Keep a record and bring it to your follow-up visits. Control your blood sugar level if you have hyperglycemia or diabetes.
- Eat a variety of healthy foods. Healthy foods include whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Eat at least 5 servings of fruits and vegetables each day. Choose foods that are low in fat, cholesterol, salt, and sugar. Eat foods that are high in potassium, such as potatoes and bananas.
- Maintain a healthy weight. Ask your healthcare provider how much you should weigh. Ask him to help you create a weight loss plan if you are overweight. Ask about the best exercise plan for you.
Call 119 for any of the following:
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have a seizure.
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
When should I seek immediate care?
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You have trouble swallowing.
- Your blood pressure or blood sugar level is higher or lower than you were told it should be.
- You have unusual or heavy bleeding.
- You fall.
When should I contact my healthcare provider?
- You have trouble having a bowel movement or urinating.
- You have questions or concerns about your condition or care.
WHILE YOU ARE IN THE HOSPITAL:
Informed consent is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
An IV is a small tube placed in your vein that is used to give you medicine or liquids.
You may need extra oxygen if your blood oxygen level is lower than it should be. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils. Ask your healthcare provider before you take off the mask or oxygen tubing.
Tests:
Monitoring:
Medicines may help improve your blood's ability to clot and stop the bleeding. You may instead need medicine to break up blood clots, or to prevent them from forming. The type of medicine you receive depends on what is causing your stroke. You may also need medicine for high blood pressure, high cholesterol, or diabetes.
Treatment:
RISKS:
You may get blood clots that can break loose and travel to your lungs or brain. You may have another stroke or go into a coma. You may be paralyzed on one or both sides of your body. You may not be able to care for yourself or live alone. You are at greater risk for falling. You may develop muscle shortening or bedsores. Even with treatment, you may have lasting problems talking, thinking, or moving your body. Without treatment, your risk for another stroke increases. This can be life-threatening.
Informed consent is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
An IV is a small tube placed in your vein that is used to give you medicine or liquids.
You may need extra oxygen if your blood oxygen level is lower than it should be. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils. Ask your healthcare provider before you take off the mask or oxygen tubing.
Tests:
- A CT or MRI may show where the stroke happened and any damage you have. You may be given contrast liquid to help your skull and brain show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- An arteriography is used to take x-rays of your arteries to look for blood flow blockage.
- Frequent blood tests may be needed while you are being treated for your stroke. These tests can tell healthcare providers if you are getting the right amount of medicine.
- A carotid ultrasound uses sound waves to show the blood flow in your carotid arteries. The carotid arteries are blood vessels in your neck that carry blood to your brain. A carotid ultrasound checks for narrow or blocked carotid arteries.
- A swallow study is used to take x-rays as you swallow certain foods and drinks. This test shows if food and liquids travel to your stomach correctly.
Monitoring:
- A neuro exam may show how well your brain works after a stroke. Healthcare providers will check how your pupils react to light. They may check your memory and how easily you wake up. Your hand grasp and balance may also be tested.
- Intake and output may need to be measured. Healthcare providers may measure how much liquid you are getting and how much you are urinating.
- A ventilator is a machine that gives you oxygen and breathes for you when you cannot breathe well on your own. An endotracheal (ET) tube is put into your mouth or nose and attached to the ventilator. You may need a trach if an ET tube cannot be placed. A trach is a tube put through an incision and into your windpipe.
- An ICP monitor measures the pressure inside your skull. A small tube is put through your skull and connected to a screen.
Medicines may help improve your blood's ability to clot and stop the bleeding. You may instead need medicine to break up blood clots, or to prevent them from forming. The type of medicine you receive depends on what is causing your stroke. You may also need medicine for high blood pressure, high cholesterol, or diabetes.
Treatment:
- You may need to wear pressure stockings or inflatable boots. The stockings are tight and put pressure on your legs. The boots have an air pump that tightens and loosens different areas of the boots. This improves blood flow and helps prevent clots.
- Physical and occupational therapy may be needed. A physical therapist teaches you exercises to help improve movement and strength, and to decrease pain. An occupational therapist teaches you skills to help with your daily activities. You will continue rehabilitation therapy after you leave the hospital.
- Bladder and bowel training helps you control when you urinate or have a bowel movement.
- Swallow therapy may help you learn safe ways to swallow to prevent coughing and choking.
- A feeding tube may be needed if you cannot swallow food or liquids.
- Thrombolysis is a procedure used to break apart clots in an artery. A catheter is guided into the artery until it is near the clot. Medicine is put through the catheter that will help break apart the clot. The clot may be pulled out of the artery during the procedure.
- Surgery may be used to remove a blood clot or to relieve pressure within your brain. You may also need surgery to remove plaque buildup from your carotid arteries.
RISKS:
You may get blood clots that can break loose and travel to your lungs or brain. You may have another stroke or go into a coma. You may be paralyzed on one or both sides of your body. You may not be able to care for yourself or live alone. You are at greater risk for falling. You may develop muscle shortening or bedsores. Even with treatment, you may have lasting problems talking, thinking, or moving your body. Without treatment, your risk for another stroke increases. This can be life-threatening.
Contact your healthcare provider or neurologist if:
Medicines:
Warning signs of a stroke: The word F.A.S.T. can help you remember and recognize signs of a stroke:
Follow up with your healthcare provider or neurologist as directed: You may need to come in for regular tests of your brain function. You may also need regular blood tests. Write down your questions so you remember to ask them during your visits.
Go to rehabilitation (rehab) as directed:
Rehab is an important part of treatment. A speech therapist helps you relearn or improve your ability to talk and swallow. You may start slowly and start doing more difficult tasks over time. Physical therapists can help you gain strength and build endurance. Occupational therapists teach you new ways to do daily activities, such as getting dressed. Therapy can help you improve your ability to walk or keep your balance. Your therapy may include tasks or movements you will need to do for everyday activities. An example is being able to raise or lower yourself from a chair.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your caregivers to decide what care you want to receive. You always have the right to refuse treatment.
- You have trouble having a bowel movement or urinating.
- You have questions or concerns about your condition or care.
Medicines:
- Medicines may help improve your blood's ability to clot and stop the bleeding. You may instead need medicine to break up blood clots, or to prevent them from forming. The type of medicine you receive depends on what is causing your stroke. You may also need medicine for high blood pressure, high cholesterol, or diabetes.
- Take your medicine as directed. Call your healthcare provider if you think your medicine is not helping or if you have side effects. Tell him if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Warning signs of a stroke: The word F.A.S.T. can help you remember and recognize signs of a stroke:
- F = Face: One side of the face droops.
- A = Arms: One arm starts to drop when both arms are raised.
- S = Speech: Speech is slurred or sounds different than usual.
- T = Time: A person who is having a stroke needs to be taken to the hospital immediately. A stroke is a medical emergency that needs immediate treatment. Some medicines and treatments work best if given within a few hours of a stroke.
Follow up with your healthcare provider or neurologist as directed: You may need to come in for regular tests of your brain function. You may also need regular blood tests. Write down your questions so you remember to ask them during your visits.
Go to rehabilitation (rehab) as directed:
Rehab is an important part of treatment. A speech therapist helps you relearn or improve your ability to talk and swallow. You may start slowly and start doing more difficult tasks over time. Physical therapists can help you gain strength and build endurance. Occupational therapists teach you new ways to do daily activities, such as getting dressed. Therapy can help you improve your ability to walk or keep your balance. Your therapy may include tasks or movements you will need to do for everyday activities. An example is being able to raise or lower yourself from a chair.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your caregivers to decide what care you want to receive. You always have the right to refuse treatment.